 SUMMARY
SUMMARY
The shift away from group homes for the developmentally disabled toward care based on shared living arrangements (SLA) is a national trend driven by economic and demographic forces. While it is widely recognized that “shared living is not for everyone,” states have different views regarding when this option is and is not appropriate. I argue that SLA-based care should be recognized as inappropriate for individuals whose ability to communicate is below the level of an average six-year-old child.
Introduction
“Shared living is not for everyone” – writes Robin E. Cooper of the National Association of State Directors of Developmental Disabilities Services.1 Having said that, she gives no explicit guidance regarding who shared living is not for. However, she does add that shared living must be “freely chosen.” Indeed, this follows from her definition of shared living as “an arrangement in which an individual, a couple or a family in the community and a person with a disability choose to live together and share life’s experiences” (italics in original).
So one guideline is implicit in her definition. Shared living is for people whose level of intellectual development enables them to make a free and informed choice. Conversely, it is not for people whose level of intellectual development is too low for them to be capable of making such a choice. In this paper I argue in favor of adopting this guideline explicitly.
The arrangements under discussion are named differently in different states. Most names are variants on either “adult foster care” or “shared living” (or “life-sharing”). The official term in Rhode Island is “shared living arrangements” (SLA). “Shared living” does convey an important aspect of these arrangements, but another aspect is no less important—care and support of the disabled person. It is not simply a matter of sharing accommodation. This second aspect is the focus of another definition that we find in an official report of the State of Vermont:
Shared living is a method of providing individualized home support for one or two adults and/or children in the home of a contracted home provider. Home providers typically have 24 hour a day/7 days a week responsibility for the individuals who live with them.2
This is why I have settled on the dual term “SLA-based care” (or “life-sharing care”).
A national trend
Study of the websites of various state governments confirms that the shift from group homes toward SLA-based care is a national trend. According to Robin Cooper, the trend is driven by “economic and demographic forces”—specifically, the recession, growing waiting lists, staff shortages, and the increasing cost of shift-staff residential programs. As increased pay and improved benefits would almost certainly eliminate staff shortages, what this all comes down to is money. Budget allocations are falling further and further below what would be required to sustain past levels of provision of places in group homes.
The difference in cost between the two types of provision is large. According to Charles Williams, head of the Developmental Disabilities Division in Rhode Island’s Department of Behavioral Healthcare, Developmental Disabilities, and Hospitals (BHDDH), state aid to group housing is 50 percent higher than state aid to shared living.3 The Vermont Report gives a much wider difference in average annual cost ($29,018 for shared living, $83,372 for group homes in 2009).
Although the NASDDDS Report attributes the trend wholly to economic and demographic factors, others have given philosophical justifications of the shift toward SLA-based care. They claim that it integrates clients more closely into the community and therefore constitutes a new stage in the process of de-institutionalization. Whether such arguments would carry weight in the absence of financial pressure is another matter.
Choice?
If the trend toward SLA-based care is driven by financial pressure, then what role is played by the element of “choice” that Robin Cooper emphasizes in her definition? No source that I have yet seen cites any data on “consumer preferences” – that is, wishes expressed by clients and their families as recorded in case files or collected by means of special surveys. People with long experience of work in group homes say that residents become attached to the places where they are (they come to feel “at home” there) and are reluctant to move. Are the extent – and especially the pace – of change required by financial targets embodied in state budgets compatible with a genuine process of free and informed choice?
Choice should apply not only to the initiation of a life-sharing arrangement but also to its termination. The State of Georgia has a guidance document on SLA-based care that includes a clause entitled “Individual Choice to Terminate Relationship” and mandating interviews conducted “by a neutral party to determine that the individual’s choice is independent of coercion from any party.”4 This is all well and good as far as it goes (provided that the individual has the requisite ability to communicate). However, what choice does the individual have concerning where to go next if the group home from which she or he came is now closed? There may be choice between one life-sharing provider and another but little or no choice regarding the SLA option itself.
Advantages and disadvantages of SLA-based care
One useful feature of the Vermont Report is its lists of advantages and disadvantages of SLA-based care, which I reproduce as an appendix.
The advantages outnumber the disadvantages 10 to 6, but from the point of view of the welfare of the disabled person this is a little misleading. Three of the advantages accrue not to the disabled individual but to the provider (nos. 2 and 4) or the state (no. 3). The remaining advantages then only slightly outnumber the disadvantages.
Note also that most of the advantages (Nos. 5—10) are about good things that may happen in a very successful life-sharing relationship, while the disadvantages refer mainly to the consequences if for any reason the relationship does not work out well. Thus, if the relationship turns sour it is the disabled person who has to move out and lose his or her home. A similar situation in a group home may be resolved by the departure of someone else.
I attach special importance to Disadvantage 3 – the greater difficulty of effective oversight in SLA-based care. In a group home other people are always around to observe and report any instances of abuse or neglect – people who are not related and therefore less inclined to cover up for one another.
Some advantages and disadvantages “cancel out”: shared living may give the disabled person more extensive contacts than those ordinarily provided by group homes (Advantages 5, 6, and 9). However, if the host family itself is socially or physically isolated (many live in rural areas), then living with them may restrict contacts and leave the person even more isolated than in a group home (Disadvantages 2 and 5).
To sum up, SLA opens up a wider range of possible outcomes than group homes. At best it makes possible a kind of loving family care that a group home can never provide. At worst, however, it entails a greater risk of undetected neglect and abuse than in the group home setting. This suggests a general guideline: those for whom SLA-based care is inappropriate are those most at risk of such an outcome.
What if anything do SLA-based and child foster care have in common?
Child foster care has been marred by many failures and abuses and has acquired a poor public reputation. An important reason why many people avoid use of the term “adult foster care” is to prevent people from associating SLA-based care of the disabled with “disreputable” child foster care. They argue that it is unfair to associate the two because children placed in foster care tend to come from broken or abusive homes and consequently have severe emotional problems with which many foster parents fail to cope. This factor does not usually apply to the disabled.
This argument has considerable weight. However, it does not follow that SLA-based care and child foster care have nothing significant in common. People with developmental disabilities, especially of a severe kind, do resemble children in important ways, and children can be difficult to look after even when they do not come from broken or abusive homes.
Some SLA providers, like some foster parents, neglect the individuals entrusted to their care for reasons that have nothing to do with the problems of those individuals. In both cases money may play too prominent a role in the motivation for providing care, and providers may display a pattern of behavior (not necessarily conscious) that favors their natural children over the person in their care.
For example, a television program highlighted a case in Pennsylvania about a developmentally disabled young woman in SLA-based care who was being abused by the young sons of her providers. Although they were quite heavy they would “playfully” jump on her and constantly demand piggyback rides from her, which gave her backache. There was no one to come to her aid while this was going on: the boys’ father was out and their mother was locked in the study at work on the computer. She could have been similarly neglected had she been a few years younger and placed in child foster care. It would not have made much of a difference.
For whom is SLA-based care inappropriate?
Apparently no one denies the existence of certain types of disabled people for whom SLA-based care is inappropriate. It is recognized that a host family cannot provide adequate care to a disabled person with complex medical needs requiring immediate access to medical professionals and advanced equipment. Nor can members of a host family be expected to exhaust and endanger themselves by attempting to cope with the most extreme forms of dysfunctional behavior.
There are, however, divergent views over where exactly the line should be drawn. Some states consider SLA-based care appropriate across the spectrum of needs, excluding only the groups mentioned in the previous paragraph but including other people with severe developmental/intellectual and/or physical disabilities. It appears to me that Rhode Island is one of these states, although I shall be very happy to be proven wrong.
Other states also exclude people with severe disabilities. South Dakota is one state that considers “Adult Foster Care” (that is what they call it in South Dakota) appropriate only for people with relatively mild disabilities. To quote their website:
The primary function of an Adult Foster Care home is to provide general supervision and personal care services for individuals who require minimal assistance in activities of daily living (ADLs), who require supervision/monitoring with the self-administration of medications, and who require supervision/monitoring of self-treatment of physical disorder. Activities of daily living are defined as any activity normally done in daily life which includes sleeping, dressing, bathing, eating, brushing teeth, combing hair, etc. …
Individuals between the ages of 18 and 59 who are capable of self-preservation in emergency situations and need supervision or monitoring in one of the following areas: 1) the activities of daily living; 2) the self-administration of medications; or 3) the self-treatment of a physical disorder.5
Thus in South Dakota individuals who require more than “minimal” assistance in activities of daily living, who cannot administer their own medication or treat their own physical disorders even with supervision and monitoring, or who would be unable to save themselves in an emergency are not considered suitable for SLA-based care.
Ability to communicate as a key criterion
Without denying the relevance of the criteria used by South Dakota, I argue that a key criterion should be ability to communicate. This is because it is especially important to exclude from SLA-based care those whose disabilities make it impossible for them to report any abuse or neglect that they may suffer and also to exercise their hypothetical right to choose whether to initiate or terminate a life-sharing relationship.
Let’s revisit Georgia’s exemplary clause on “individual choice to terminate relationship” and try to apply it to a physical adult who in mental terms remains a toddler, either completely non-verbal or with a vocabulary of a dozen or so words. “When an individual indicates a desire to terminate services from a Host Home provider” (how? by running away?) “the individual will be interviewed by a neutral party” (but he or she doesn’t know how to answer questions). “The individual’s support coordinator … will interview the individual’s legal guardian (if any) and/or any representative who has been formally or informally designated by the individual” (but the individual is incapable of designating a representative, even informally).
Some may say that it suffices if the right to choose is exercised on the individual’s behalf by a guardian. Guardians who as parents or other close relatives used to care for the individual and who visit the individual frequently are indeed the best persons to detect signs of any abuse that may have occurred and to take decisions on the individual’s behalf. However, when communication deficits are very severe even parents may be unable to assess a situation reliably. For instance, it is hard even for them to judge whether unresponsiveness and withdrawal result from distressing experience or lack of interaction (a form of neglect) or whether they have some harmless cause. Moreover, when the original guardians lose the ability to perform the duties of guardianship or die the new guardian may be a relative who is unable to visit so frequently or – even worse – some court-appointed lawyer who does not know or care very much about the individual and hardly ever visits. Or there may be no guardian at all: the disabled person may become a ward of the state.
How is ability to communicate to be measured? A common measure of general intellectual ability for the developmentally disabled is mental age. Ability to communicate usually but not always corresponds to mental age. Some people’s ability to communicate is impaired solely by physical disabilities (or perhaps they could communicate adequately, but only with the aid of advanced equipment that is too expensive or not yet widely available). Autism also impairs communication. So mental age is not quite what we need. We need not the individual’s mental age but the mental age that corresponds to the individual’s ability to communicate – that is, the average age of children without disabilities whose ability to communicate is at the same level as that of the individual. We could call this the individual’s “communicative age.”
Below what limit in terms of communicative age should we recognize an individual as especially vulnerable and therefore unsuitable for SLA-based care?
According to the Encyclopedia of Mental Disorders, the “mentally retarded” (in deference to the current demands of political correctness I shall switch that to “developmentally disabled”) are a class of individuals with IQ below 70 and mental age below 12 years. They make up about 2% of the population and are divided into four subgroups on the basis of degree of disability: mild, moderate, severe, and profound. The mildly disabled, with IQ in the range 50—69 and mental age in the range 8—11 years, account for 85% of the whole class. The moderately disabled, with IQ in the range 35—49 and mental age in the range 4—7 years, contribute another 10%. The severely and profoundly disabled, with IQ below 35 and mental age below 4, make up the remaining 5%.
I suggest that we set the limit in such a way as to recognize as unsuitable for SLA-based care all the severely and profoundly disabled and a section of the moderately disabled – that is, individuals with a mental (more precisely, communicative) age below 6 years. This would cover somewhat less than 10% of the whole class (perhaps 8%), because people with a mental age of 6—7 outnumber people with a mental age of 4—5.
Who would assess an individual’s communicative age? I suggest that the parents (or other family caregivers) and the caregivers at the day program attended by the individual (if any) be asked to estimate his or her communicative age. If both give ages below 6 years that would decide the matter in one direction; if both give ages of 6 years or above that would decide the matter in the other direction. Only if one assessment is below 6 years and the other is 6 years or above would the matter be referred for a professional assessment.6
Do we need formal criteria?
Some people prefer not to classify the developmentally disabled on the basis of formal criteria, especially if these criteria focus on degree of disability. They say that they prefer to treat people as individuals.
This sounds very nice. Formal rules do have their drawbacks. They often fail to make provision for exceptional cases. But in the real world they are a lesser evil. A lack of formal rules can easily result in – and help cover up – a financially driven neglect of vital needs.
People have unique individual needs. But they also have needs that they share with other members of a certain class. For example, blind children need to be taught braille and deaf children need teachers able to converse with them in sign language. If they were not classified as blind or deaf but regarded only as unique individuals with a right to be placed in “the least restricted environment” then those needs would probably go unmet.
In the same way, people with severe developmental disabilities have special needs for care and protection that they share with one another but do not fully share even with people fortunate enough to have only mild developmental disabilities. Due attention to these class-specific needs is quite compatible with efforts to meet their individual needs as well – to provide each individual with his or her favorite toys, stuffed and squeaky animals, games, foods, videos, songs, and other sensory experiences.
If decisions about which needs to meet and how to meet them were made solely by competent professionals concerned only with the welfare of their charges, then we might just leave things to them and not burden them with formal rules.
Unfortunately that is not the situation. Financial pressure is a powerful influence on decision making. In the absence of formal criteria that pressure may inflict special harm on the severely disabled because it is their care that involves the highest per capita costs. It may well seem to decision makers concerned primarily with costs that this is where the biggest savings are to be made.
To be specific, unless people with severe developmental disabilities are explicitly deemed unsuitable for SLA-based care the financial pressure to place them in such care will be even stronger than the pressure to place the mildly disabled there. As Mr. Williams informed the Warwick Beacon: “On average the annual savings for an individual in SLA over group housing is $19,400, with that number increasing depending on the severity and dependence on services” (my italics).7
So yes, we do need formal criteria. Compliance with formal criteria can be verified. That makes it possible for us to hold our state officials accountable. If we could have implicit trust in them we would not need formal criteria. But we cannot trust them. In fact, it is our civic duty to distrust them. The principle of organized distrust of government lies at the core of American constitutional thought. That is its main contribution to the progress of civilization.
Notes
1. In a report entitled Shared Living: A New Take on an Old Idea, prepared for the Arizona Developmental Disabilities Planning Council and issued in Spring 2013 (henceforth “the NASDDDS Report”). Available for download at the site of the NASDDDS. If you have trouble downloading it (as I did) e-mail me at sshenfield@verizon.net and I’ll send it to you.
2. Shared Living in Vermont: Individualized Home Supports for People with Developmental Disabilities 2010. State of Vermont, Division of Disability and Aging Services, Department of Disability, Aging and Independent Living (henceforth “the Vermont Report”). Accessible at www.dail.vermont.gov. The inclusion of disabled children as well as adults here confuses the distinction between shared living and foster care.
3. Daily rates of $162 versus $109. See: Kelcy Dolan, “Budget concerns shift perspective from group homes to shared living,” Warwick Beacon, January 21, 2016 (http://warwickonline.com/stories/budget-concerns-shift-perspective-from-group-homes-to-shared-living,108733).
4. Process for Enrolling, Matching, and Monitoring Host Home/Life-Sharing Sites for DBHDD Developmental Disabilities Community Service Providers, 02-704, Clause F (https://gadbhdd.policystat.com/policy/832301/latest/).
5. State of South Dakota, Department of Human Services, Division of Developmental Disabilities, page on Adult Foster Care (https://dhs.sd.gov/dd/adultfc.aspx).
6. The assessment could be carried out at the Children’s Neurodevelopment Center (formerly the Child Development Center) at Hasbro Children’s Hospital in Providence – if they agree to count developmentally disabled adults as “children”!
7. Source as for note 3.
Appendix. Advantages and disadvantages of shared living according to the Vermont Report
Advantages
1. Shared living offers a wide variety of flexible options to meet the specific needs of individuals.
2. The “difficulty of care” payment to a home provider is exempt from federal and state income tax.
3. Shared living, on average, has a lower per diem cost than other types of twenty-four hour a day home support, such as staffed living and group homes.
4. Shared living offers an opportunity for support workers to earn income while working out of their home.
5. Home providers may support and facilitate contact with the individual’s natural family.
6. A home provider’s extended family and friends often become the “family” and friends of the individual who lives with them. The individual may have a chance to share holidays and go on vacations with the home provider.
7. Consistency in supports offered in a home setting is good for individuals who are highly medically involved or have other complex support needs. There is a high probability that individuals in shared living who are terminally ill will receive end of life care at home.
8. Shared living often leads to long-term stability and consistency in the individual’s life as many home providers become life-long companions to the individual who lives with them.
9. Home providers often provide the necessary transportation that helps an individual get to places he or she needs or wants to go.
10. Shared living offers targeted skill development that affords a safe and measured approach toward more independent living
Disadvantages
1. Individuals receiving services from agencies may become comfortable with this option. It can therefore be programmatically, emotionally and fiscally challenging for individuals to “graduate” out of shared living to more independent supervised living.
2. Shared living can limit an individual’s exposure to other people and places outside the home or to what the home provider experiences.
3. There may be fewer independent or external eyes on the individual, thus reducing opportunities for oversight.
4. Because the home must be the primary residence of the home provider, if the specific living arrangement does not work it is the individual that has to move out.
5. Given limited public transportation and the rural location of many shared living homes, an individual’s access to alternative transportation options are often limited.
6. Home providers may be challenged when, as employers, they are required to hire, train and supervise workers to provide respite, community supports and/or employment supports to the individual living with them.
]]>
 Update (February 4, 2016). In response to public concern the BHDDH has requested supplemental funding in order to obviate the need to implement its previous transfer plan, adopted reluctantly under pressure from the house finance committee. The governor has granted the request for supplemental funding. The intention now is to aim at the transfer to adult foster care (“shared living arrangements”) of only 100 individuals, not “up to 300.” These individuals will be selected from group homes run by private agencies as well as state-run group homes. There is no longer any deadline for meeting the target and the usual safeguards will be used. Under these conditions the risk to residents is greatly reduced and the issue can be regarded as resolved.
Update (February 4, 2016). In response to public concern the BHDDH has requested supplemental funding in order to obviate the need to implement its previous transfer plan, adopted reluctantly under pressure from the house finance committee. The governor has granted the request for supplemental funding. The intention now is to aim at the transfer to adult foster care (“shared living arrangements”) of only 100 individuals, not “up to 300.” These individuals will be selected from group homes run by private agencies as well as state-run group homes. There is no longer any deadline for meeting the target and the usual safeguards will be used. Under these conditions the risk to residents is greatly reduced and the issue can be regarded as resolved.
In the January 14, 2016 issue of The Providence Journal, Jennifer Bogdan reports that “the [Rhode Island] Department of Behavioral Healthcare, Developmental Disabilities and Hospitals (BHDDH) plans to move up to 300 adults with developmental disabilities from group homes into shared residential living arrangements by the end of March.”
What is a “shared residential living arrangement”? It means that a disabled individual lives with a family that volunteers to accommodate and look after him or her and is paid for doing so. Another clearer term for such an arrangement is “adult foster care.” However, this term may be used to refer to group homes as well as family homes, so a better term is “family adult foster care.”
The report continues: “Maria Montanaro, the agency’s director, said it’s a model the state should be moving toward regardless of whether there is a budget crisis.” Nevertheless, it is clear that the main appeal of family adult foster care to policy makers is the fact that it is cheaper.
In fact, as professionals with long experience in this field have told me, no single model of care is suitable for all disabled people. It is therefore important to maintain a balanced mix of facilities, and group homes are an essential part of this mix.
Criteria for foster care
When is family adult foster care an appropriate model and when is it inappropriate? It depends on the severity of the disabilities. Beyond a certain point on the scale of severity, an ordinary family will simply lack the skills, time, energy, and other resources needed to provide the disabled person with an adequate standard of care. (This is not to deny the existence of special cases in which family members happen to be professionals with relevant knowledge and experience.) By intending to keep two specialized group homes in operation, the BHDDH implicitly acknowledges that some disabled people have needs that cannot easily be met in family adult foster care. The question is where exactly the line should be drawn.
I have searched for documents that specify criteria for placing a disabled adult in family adult foster care. I did not find such a document on a federal government website, but some state government sites are more helpful. Here are the criteria specified on one of these sites:
1. The individual must require minimal assistance in activities of daily living (dressing, bathing, eating, using the toilet, brushing teeth, combing hair, cutting nails, etc.) or need supervision or monitoring in these activities, in the self-administration of medications, or in the self-treatment of a physical disorder.
2. The individual must be capable of self-preservation in emergency situations.
In other words, members of the foster family are not expected to provide more than “minimal” assistance to the disabled person, however that may be defined. They are not expected to administer medications or treat a physical disorder, but only to supervise or monitor the disabled person doing so. The disabled person must be able to vacate premises in the event of a fire or other emergency. All this requires that the degree of disability must be moderate.
How severely disabled are the people to be transferred?
How severe are the disabilities of the residents in Rhode Island’s state-run group homes? I do not have detailed data, but all indications are that the average level of disability is high. A retired informant who worked in these homes for thirty years tells me that about half of the residents are confined to wheelchairs; many have severe mental disabilities and quite a few are unable to speak. (Others communicate by sign language. Would members of foster families be required to learn sign language?) In the group homes they receive round-the-clock care from well-trained dedicated staff.
We must also bear in mind that the figure for the number of residents to be transferred to foster care by the end of March – 300 – was determined by the amount of money that has to be saved in order to close a budget shortfall. It is not an estimate of the number of residents whose disabilities are sufficiently moderate to be safely placed in foster care. The 300 may therefore include people with severe physical and/or mental disabilities. In fact, Ms. Montanaro clearly implies that this is so when she states that “matches have been found across the spectrum of needs.”
It is true that volunteer families are vetted for suitability. But how reliable is the vetting procedure? Does it effectively exclude people whose motives are purely financial? Moreover, the planned transfers are to be made under strong time pressure. According to Montanaro 100 new families have already been found and 200 more are needed. It may well prove necessary to relax the requirements set for foster families in order to meet the deadline.
These circumstances justify fears that many of the disabled people hastily placed in foster care will be neglected or abused. True, neglect and abuse also occur in group homes. However, in the group home context there are always others around who may observe and report abuses. Awareness of this deters many care staff who might otherwise mistreat residents. In a foster home the disabled person is more isolated and abuse may remain undetected for a long time (unless inspections are frequent, intrusive, and unannounced).
Not many of those who are to be removed from their familiar environment to foster care still have relatives who visit regularly and look out for their welfare. Most are wards of the state. This makes them especially vulnerable.
The question of stability
The Providence Journal quotes Montanaro as saying that foster care “is preferable in part because group homes tend to have frequent staff turnover” while foster care “can offer more stable relationships.”
The first thing that a careful reader of this sentence notices is that Montanaro is comparing like with unlike – the high staff turnover that group homes actually have with the stability that foster care can offer. This is dishonest. As the expression “tend to” implies, group homes do not always suffer from high turnover. It depends on the interrelated factors of morale and pay. State-run group homes, where workers are relatively well paid, may well have much lower turnover than group homes run by private agencies, where pay is only a little above the minimum wage.
Nor is foster care necessarily stable. Individuals who are difficult to look after may have to be moved repeatedly from one family to another. Even a family that does achieve a stable and caring relationship with their disabled ward will have to be relieved of their responsibilities when their circumstances change or as they age. A disabled person needs care for the whole of his or her natural life.
Moreover, stability is not a matter solely of relationships with caregivers. Even with fairly high staff turnover a group home offers a measure of environmental and institutional stability. A caregiver may leave, but the person remains in a familiar physical environment and the daily routine probably also remains the same. Disruption is less total than that involved in a move from one family to another.
The question of choice
The Providence Journal also quotes Ms. Montanaro as saying: “We’re not forcing people into these arrangements.” Are the candidates for transfer really in a position to make a free and informed choice?
We have to give separate consideration to two cases – that in which the person’s mental and linguistic abilities suffice for a conversation about alternative residential and care arrangements and that in which the person’s disabilities make such a conversation impossible.
Free choice requires that the BHDDH social worker conducting the conversation should exert no psychological pressure. There must be no sign that she prefers one possible answer to another. In reality she does have a preference because she herself is under pressure to help meet the target number of transfers. How effectively does she conceal this preference?
Informed choice requires that the social worker explain not only the possible advantages and benefits of foster care but also its possible disadvantages and risks. And yet her boss, Maria Montanaro, is unwilling to give the state legislature a balanced assessment that acknowledges these disadvantages and risks.
It is especially difficult to ensure that force is not used against those incapable of speaking for themselves. What methods will be used to give them a choice? Generally speaking, people with severe developmental disabilities, provided that they are not being abused, show a strong desire to stick to familiar routines and remain in a familiar environment. Change upsets them.
A couple of suggestions
Even if the BHDDH is unwilling to give up the idea of transferring disabled residents of group homes to family foster care, moves could be made in this direction with less risk to the wellbeing of the disabled.
I suggest, first, that candidates for transfer be selected from all group homes, including those run by private agencies, and not only from state-run group homes. Expansion of the pool would make it possible to choose more individuals who had only moderate disabilities and were therefore really suitable for foster care.
Why are state-run homes being specially targeted for closure? The explanation seems to lie in the ideological animosity that many of our politicians feel for public institutions. This is shown, for example, in changes that the Rhode Island legislature made to the budget proposed by the state governor for the current financial year (2016). The governor had recommended $46.5 million for the state-run facilities, but the legislators switched $4 million of this sum (almost 9%) to “assistance and grants” to private agencies. (See here. The state-run homes come under Rhode Island Community Living and Supports (RICLAS), which forms part of the BHDDH.)
My second suggestion is to take an experimental approach, first trying the transfer to foster care on a small scale and assessing the results before committing irreversibly to the strategy. The 300 individuals whose transfer is contemplated would be identified, a representative sample of (say) 20 of them selected and placed with foster families, and the results assessed at three-month intervals for a year, without yet closing any group homes. Further decisions would then be made in light of the results of the experiment. If the experiment is a failure then the sampled individuals can be returned to their group homes. If group homes are closed before the results of the transfer to foster care are known, where are disabled people to go if foster placements prove unsatisfactory? There is reason to fear that they may end up in some mental hospital.
Just to save a little money
For what are the group homes being closed and the wellbeing of their residents placed in jeopardy? The aim of the exercise is “to close a projected $6 million budget shortfall.” This may seem a lot of money to some people, but in terms of total expenditures of state government it is loose change — a mere 0.07% of the FY 2016 operating budget. Fifty times as much ($300m) is being spent in FY 2016 on administering the state lottery.
The way in which a society treats its weakest, most defenseless and vulnerable members is a good measure of its level of civilization — or barbarism.
]]>
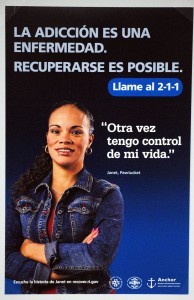 The Departments of Health (HEALTH), Behavioral Healthcare, Developmental Disabilities and Hospitals (BHDDH) and the Anchor Recovery Community Center held a press conference today to announce the launch of a new media campaign, “Addiction is a Disease. Recovery is Possible.”
The Departments of Health (HEALTH), Behavioral Healthcare, Developmental Disabilities and Hospitals (BHDDH) and the Anchor Recovery Community Center held a press conference today to announce the launch of a new media campaign, “Addiction is a Disease. Recovery is Possible.”
The ads cover television, radio, billboards and the sides of buses. There is a website. The powerful ads feature eight local men and women who tell their stories of addiction and recovery. Though many share their personal stories of addiction, one woman, Elise, speaks from the point of view of a mother who lost two sons to overdose.

Holly Cekala, executive director of RICAREs (the group that staged a “Die-In” outside the State House earlier this week) pointed out the wide range of ages, races and economic level of those in recovery and told me that the community she serves, and is a part of, is the most diverse community there is. Addiction, it seems, does not discriminate.
Anchoring the event and introducing the speakers was Jim Gillen, Director of Recovery Services at the Providence Center / Anchor Community Center. Gillen has been in long term recovery since 1998 and “As a result, my life is banging, let me tell you,” he said to the audience, “It’s the reason that I’m employable, it’s the reason that I pay taxes, that I drive with a license and insurance… and I vote.”
Dr. Michael Fine, director of HEALTH, said that the point of this campaign is to let “every single Rhode islander know that addiction is a disease.” This is a “campaign to bring Rhode Islanders together.”
There were 232 overdose deaths in Rhode Island last year. People have already died this year. “With each death,” says Dr. Fine, “a piece of Rhode Island dies.”
Dr. Fine revealed that another aspect of this campaign is designed to raise awareness among doctors and others with the power to prescribe opiates about their responsibility in curbing this epidemic, as well as bringing more accountability to the pharmacies that fill the prescriptions. “We need to change our prescribing behavior,” said Dr. Fine.
Linda Mahoney of BHDDH sees this campaign as a means of combating the stigma that addiction carries. She commended the eight people appearing in the ads for having the courage to face this stigma head on in an effort to change the hearts and minds of the wider community. It takes courage, said Mahoney, “to come out professionally and publicly and say, ‘I know I was sick. I got better and there is still work to do.’”
“The idea is to overcome stigma, to treat addiction as a disease like any other disease,” said Mahoney.
Jonathan, one of the eight featured in the ads, started with a joke, “When I was told that this campaign would mean having my face plastered on the side of a bus, I said that this wouldn’t be the first time I was plastered on a bus.” But he soon turned serious. His was a story of addiction that lead to crime and estrangement from friends and family.
It ultimately led to his death, but he was saved by an injection of Narcan. Waking up in the hospital, Jonathan’s first thought was to score more drugs, but he learned that there were people out there who “loved me more than I loved myself.”
Jonathan has been in recovery for 19 months. He is repairing his relationship with his family, has a job and is paying the debts he accrued during his addiction. Still, addiction haunts him. On Wednesday he attended a funeral for a 22-year old friend, one of the first overdose deaths in 2015.
Elise spoke next. She is a nurse who has worked in recovery since 1998. Her son Paul died at the age of 22 in 2004, and her son Teddy died at age 30 in 2010. “Who would have thought it would happen to me?” Elise asked, “You can’t have your blinders on.”
‘We can’t arrest ourselves out of this problem,” said Dr. Fine during the question and answer session, observing that addiction is a medical, not law enforcement problem. Jim Gillen, wrapping up the event, seemed to concur. “We may have lost the war on drugs,” he said, “but we will win the war on addiction.”
Below are all eight videos produced for the campaign.
]]>